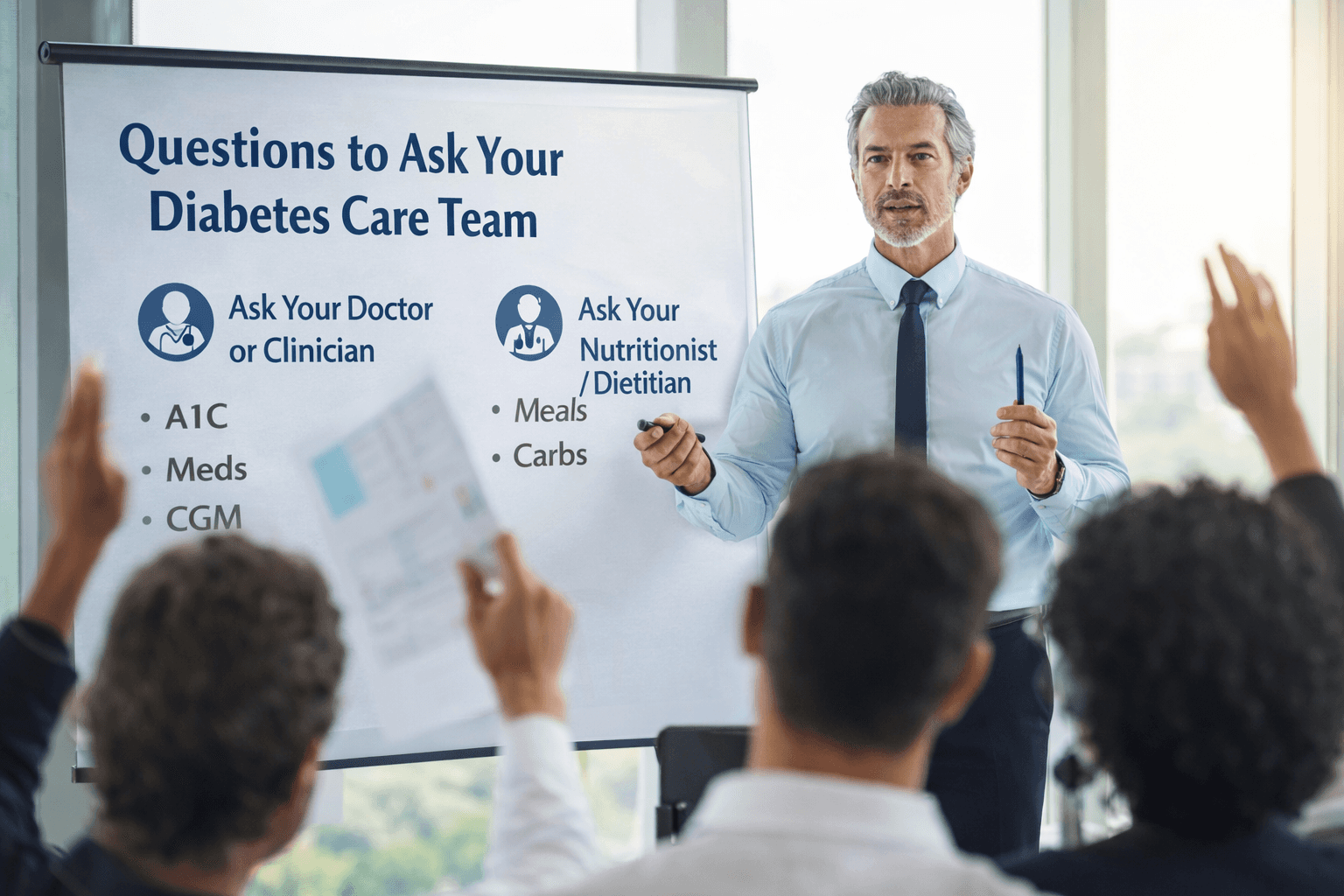
Discover the top questions to ask your diabetes care team—your doctor, clinician, or nutritionist so you can understand your numbers, personalize your plan, and leave your next visit with clear, actionable steps.
Heald Membership: Your Path to Diabetes Reversal
Table of content
A good diabetes plan isn’t just what you do at home—it’s also the quality of support you get from your healthcare team. The right questions can help you understand your numbers, reduce confusion about food and exercise, and make sure your treatment plan matches your real life.
This Patient Guide is a consolidated checklist of the most important questions to ask at your next visit—whether you’re meeting with your doctor/clinician or your nutritionist/dietitian. Bring it on your phone, print it, or copy it into a notes app so you can capture answers in the moment.
If you’re starting from scratch and want to understand your risk level first, begin with Calculate Your Diabetes Risk.
Before Your Appointment: Quick Prep (5 minutes)
These quick steps make your visit more productive:
Write down your current meds and doses, supplements, and any side effects.
Bring recent lab results (A1C, fasting glucose, lipids) if you have them.
Track 3–7 days of meals, movement, sleep, and symptoms (even simple notes help).
List your top 2 goals (examples: lower A1C, lose 5–10 lbs, reduce cravings, improve blood pressure).
For help building the habit foundation before your appointment, see How It Works.
10 Questions to Ask Your Doctor or Diabetes Clinician
Use these to clarify your diagnosis, treatment plan, and safety:
What do my numbers mean right now? (A1C, fasting glucose, time-in-range, blood pressure)
What’s my goal range—and why? What should my A1C or daily glucose targets be?
Is my diagnosis prediabetes or type 2 diabetes? What stage am I in, and what’s realistic in 3–6 months?
What complications should I screen for—and how often? Eyes, kidneys, nerves, heart health, and labs.
Which medications are best for my situation? Benefits, risks, cost, and what to monitor.
What side effects should I watch for? And what should I do if they happen?
Can lifestyle change reduce my meds over time? What does safe step-down look like?
Should I use a CGM or glucose meter? If yes, how often should I check and what patterns matter?
How should I manage diabetes with high blood pressure or cholesterol? Do targets change?
What’s the plan if I get sick, travel, or change routines? (sick-day rules and adjustments)
If you’re actively working on lifestyle change and remission strategies, pair this visit with Diabetes Reversal Guide and Diabetes Prevention Program.
10 Questions to Ask Your Nutritionist or Dietitian
Use these to get a plan that’s realistic, personalized, and sustainable:
What eating pattern fits my goals best? (balanced plate, Mediterranean, lower-carb—based on my labs and lifestyle)
How much protein should I aim for daily? And what are easy protein options?
Which carbs work best for me? How do fiber and portions affect my glucose?
How should I build meals to reduce spikes? (protein/fiber first, timing, and simple plate templates)
What are “go-to” meals and snacks you recommend for my schedule?
How do I handle cravings and emotional eating? Tools for stress eating and late-night snacking.
What should I eat before/after workouts? Especially if I’m walking after meals or strength training.
How can I eat out without guessing? Ordering strategies, swaps, and portion cues.
What should I do if I’m also managing high blood pressure? Sodium, hydration, and heart-friendly choices.
How do we track progress? What should I monitor weekly and how often should we adjust?
To support the nutrition plan with movement that improves insulin sensitivity, visit Fitness & Exercise.
During the Visit: Make Sure You Leave With a Plan
Before you end the appointment, ask:
“What are my top 3 priorities until the next visit?”
“What should I track, and how often?”
“When do we follow up—and what would count as success?”
If you want ongoing support for habit-building, structured guidance, and progress tracking, explore Membership and the HealD approach to sustainable change.

Sandeep Misra is the Co-Founder and Chief Growth Officer at Heald, where he leads growth strategy and partnerships for data-driven programs focused on diabetes reversal and metabolic health. He brings over two decades of experience across healthcare technology, population health, and enterprise partnerships, having held senior leadership roles at AWS, Rackspace, and NTT Data.
Popular Blogs
Comments