Heald Membership: Your Path to Diabetes Reversal
Table of content
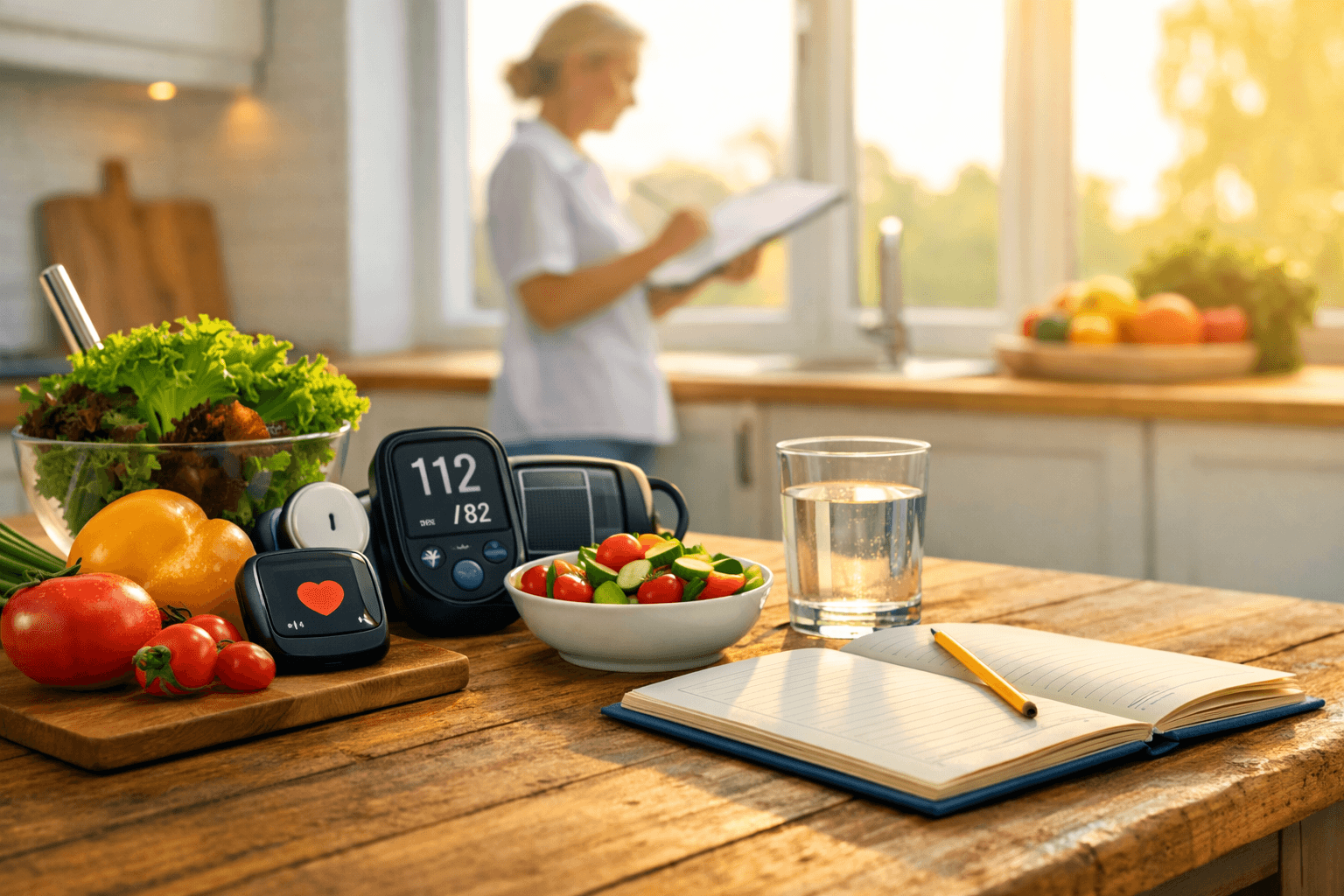
If you’ve been told you have prediabetes, type 2 diabetes, or high blood pressure alongside diabetes, it can feel like your health is now defined by numbers—A1C, fasting glucose, and blood pressure readings. The good news: for many people, prediabetes can be reversed, and type 2 diabetes can often be put into remission through sustainable lifestyle changes—especially when you treat the root cause (insulin resistance) and build habits you can maintain long-term.
This pillar guide consolidates the major sections from these HealD resources into one roadmap:
Type 2 reversal without medication (remission-focused)
Prediabetes reversal (diagnosis + action plan)
Lifestyle changes for hypertension + diabetes (single plan for both)
Start here: Take the Calculate Your Diabetes Risk assessment, then use this guide as your step-by-step reference.
1) First, understand what you’re reversing (and what “reversal” really means)
Type 1 vs. Type 2: why the distinction matters
Type 1 diabetes is autoimmune and requires lifelong insulin therapy (it can’t be prevented or reversed).
Type 2 diabetes is primarily metabolic: your body still makes insulin, but doesn’t use it effectively (insulin resistance).
Insulin resistance in plain language
Think of insulin like a “key” that helps glucose enter your cells for energy. With insulin resistance, the “lock” becomes less responsive, glucose stays in the bloodstream, and the pancreas works overtime—until it can’t keep up.
“Cure” vs. remission: the real goal
There isn’t a permanent “cure” for type 2 diabetes, but remission is an achievable target for many—meaning blood sugar returns to a healthy range without diabetes medication, maintained by lifestyle. Remission isn’t a finish line; it’s a state you maintain with the habits that got you there.
2) Prediabetes: diagnosis, numbers, and why acting early matters
Prediabetes is a fork in the road, not a dead end—and it often comes with few or no obvious symptoms, which is why testing matters.
What the key numbers mean (A1C + fasting glucose)
Typical ranges used in the guide include:
Normal: fasting glucose ≤ 99 mg/dL and A1C < 5.7%
Prediabetes: fasting glucose 100–125 mg/dL or A1C 5.7%–6.4%
Type 2 diabetes: fasting glucose ≥ 126 mg/dL or A1C ≥ 6.5%
Tests used to diagnose prediabetes
Common tests include the Fasting Plasma Glucose (FPG) test and the A1C test.
A realistic target that moves the needle
Prediabetes reversal can be driven by consistent, achievable goals, including modest weight loss (~5–7%) and regular movement you can sustain.
3) The “one plan” approach: why diabetes and high blood pressure often show up together
If you’re managing diabetes and hypertension, you don’t need two separate complicated playbooks. These conditions often share metabolic roots—especially insulin resistance—and can reinforce each other over time.
Insulin resistance and elevated glucose can damage blood vessels and reduce flexibility, increasing pressure demands on the heart.
The relationship can become a feedback loop; a large share of people with diabetes also have high blood pressure.
The solution is a single foundation built on five pillars: nutrition, exercise, weight management, sleep, and stress.
4) Nutrition: flexible templates that reduce spikes and support your heart
The non-negotiable: whole foods first
Across successful approaches, the common thread is moving away from highly processed foods and toward whole, nutrient-dense foods that support steadier glucose and better blood pressure.
DASH + Mediterranean = strong starting frameworks
Both the DASH and Mediterranean patterns are highlighted as flexible templates that emphasize fruits, vegetables, whole grains, and healthy fats while limiting excess salt/sugar—supporting both blood pressure and glucose goals.
Low-carb vs. Mediterranean: which is better?
There’s no one “best” diet for every body. People achieve improved glucose control and remission with different frameworks; the best one is the one you can follow long-term with your care team’s support.
Prediabetes food priorities
A practical prediabetes eating strategy includes:
Eat more: lean protein, healthy fats, fiber-rich vegetables, and complex carbs
Limit: sugary drinks and highly processed/refined carbs
Stabilize with structure: meal timing + sensible portions to avoid “rollercoaster hunger”
Mindful eating + portion awareness
How you eat matters too—mindful eating helps reduce automatic or emotional eating patterns and makes portion control feel more natural and sustainable.
5) Movement: consistency beats intensity (and helps both glucose + BP)
Exercise doesn’t have to be extreme to be effective. The guidance emphasizes building a routine you’ll repeat:
Cardio you enjoy (walking, cycling, swimming, dancing)
Strength training to improve insulin sensitivity and metabolic health
Low barrier starts (ex: a short walk after meals) to build momentum
A key theme across the content: don’t chase perfection—start small, stay consistent, and choose activities that feel doable and even fun.
Internal resource: Explore workout guidance inside Fitness & Exercise.
6) Sleep + stress: the quiet multipliers
Stress and sleep aren’t “soft” topics—they directly affect physiology.
Stress hormones like cortisol can raise blood sugar, and chronic stress can push blood pressure higher while draining willpower.
Poor sleep can reduce insulin sensitivity and disrupt appetite hormones, making nutrition consistency harder.
Start simple: protect a consistent bedtime window, reduce late stimulants, and add small daily stress reducers (walk, breathing, connection).
7) Weight loss: why it can “reset” metabolic function
Weight loss is presented as one of the strongest levers for improving insulin resistance—often with meaningful impact even at moderate levels (commonly discussed as ~5–10%). Excess fat around organs like the liver and pancreas can interfere with insulin function; reducing it helps the system work better.
8) Tracking and feedback: stop guessing and start learning your patterns
Glucose monitoring (prediabetes + type 2)
Tracking helps you connect cause and effect—what meals, movement, stress, and sleep do to your numbers—so you can personalize your plan instead of following generic rules.
Internal resource: Learn more in Tools & Technology.
Home blood pressure monitoring (if hypertension is part of your picture)
Best practices highlighted include measuring at the same time daily (often morning), sitting quietly beforehand, and using a validated monitor with your clinician’s guidance.
9) Safety and medical partnership (especially if you want fewer meds)
Very low-calorie diets (VLCDs): promising but not for DIY
VLCD-style approaches have been associated with remission outcomes in research contexts, but they’re described as medically supervised and hard to maintain, and not a default long-term solution.
Intermittent fasting: can help some, risky for others
Fasting may support medication reduction for some people, but it can be risky—especially if you’re on meds that lower glucose (like insulin). Do this only with medical supervision.
“Medication-free” should never mean “doctor-free”
If you’re aiming to reduce or eliminate medication, the guidance strongly emphasizes working with a medical team for safe monitoring and adjustment—medication can also be a temporary bridge while habits take root.
10) Make changes stick: mindset, support, and small wins
The content repeatedly reinforces behavior strategy over willpower:
build support (family, friend, coach, community)
focus on small wins to create momentum
create an accountability system via simple tracking

Sandeep Misra is the Co-Founder and Chief Growth Officer at Heald, where he leads growth strategy and partnerships for data-driven programs focused on diabetes reversal and metabolic health. He brings over two decades of experience across healthcare technology, population health, and enterprise partnerships, having held senior leadership roles at AWS, Rackspace, and NTT Data.
Popular Blogs
Comments